Educational Resources
Aloha,
We are pleased to provide you with access to the data gathered during this study. It is essential to understand that these metrics were acquired in a research environment at one moment in time, and thus are not guaranteed to hold any clinical significance or relevance to your health. The results provided in your personal dashboard do not provide a conclusive diagnosis, but can be useful to share and discuss with your primary-care physician in order to monitor your overall health and well-being. It is crucial to recognize that even if your metrics fall outside of recommended target ranges, this alone does not necessarily imply a state of illness. Rather, these metrics may indicate a potential concern that you should discuss further with your healthcare provider.
If you have any other inquiries or concerns about these metrics, you should also seek guidance from your healthcare professional. They possess the expertise and knowledge necessary to interpret these metrics within the context of your overall health and medical history. While these data are valuable for research purposes, they should not replace personalized medical advice or clinical evaluations conducted by trained healthcare providers. Your well-being is of utmost importance, and it is always prudent to consult with a healthcare expert for a comprehensive understanding of your health status.
Mahalo,
The MauiWES team
Basic Physiological Assessments:
Blood Pressure
Blood pressure refers to the force exerted by circulating blood against the walls of blood vessels. It is measured in millimeters of mercury (mmHg) and consists of two components: systolic pressure, which represents the force when the heart contracts and pumps blood, and diastolic pressure, which signifies the pressure when the heart relaxes between beats. Understanding blood pressure is crucial as it serves as a key indicator of cardiovascular health. Elevated blood pressure levels can impose strain on the heart and blood vessels, predisposing individuals to conditions such as coronary artery disease and stroke. Please keep in mind your results here are not a substitute for a clinical diagnosis, but rather serve as supportive information for your primary care physician to monitor your health and well-being.
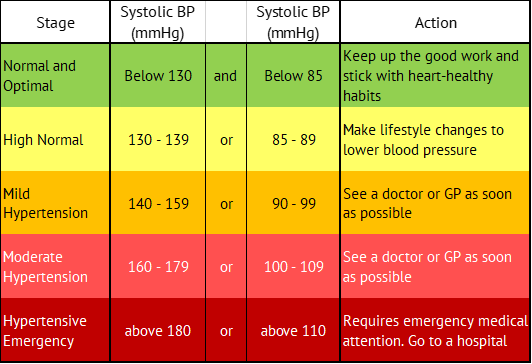
The recommended target ranges for Blood Pressure are:
It’s important to note that fluctuations in blood pressure are normal. However, persistent high or low blood pressure should be evaluated by a healthcare professional to identify any underlying causes and determine the appropriate course of action. Regular monitoring and lifestyle modifications, such as maintaining a healthy diet, exercising regularly, managing stress, and avoiding tobacco and excessive alcohol consumption, can help maintain optimal blood pressure levels. It’s essential to monitor blood pressure regularly and consult with a healthcare professional for personalized advice.
Body Mass Index
Body Mass Index (BMI) is a measure of body fat based on an individual’s weight and height. It’s calculated by dividing weight in kilograms by the square of height in meters (kg/m²). Monitoring BMI is crucial as it provides a quick assessment of one’s weight status relative to their height, aiding in the identification of potential health risks.
BMI serves as an indicator for various health complications associated with weight. An underweight BMI (less than 18.5 kg/m²) can indicate malnutrition, weakened immunity, and developmental issues, while individuals with a high BMI (over 25 kg/m²) are at risk of conditions like cardiovascular diseases, type-2 diabetes, hypertension, and certain cancers. Regular tracking of BMI allows for early intervention and tailored health plans to mitigate risks associated with both low and high BMI. It enables healthcare professionals to offer appropriate guidance, lifestyle modifications, and preventive measures to optimize health and reduce the likelihood of weight-related health complications. In considering your BMI, it’s important to consider your personal circumstances. Specifically, BMI may overestimate body fat in athletes and others who have a muscular build, while it may underestimate body fat in older persons and others who have lost muscle. Additionally, the ethnic and genetic background can influence the association between your BMI and health risks.
Body mass index (BMI) is a useful measure for your health in terms of your relative size. It is calculated from your height and weight, dividing your weight in kilograms by your height in meters squared (m2). BMI is an estimate of body fat and a good gauge of your risk for chronic diseases that can occur when more body fat is present. The higher your BMI, the higher your risk for diseases such as heart disease, high blood pressure, type 2 diabetes, gallstones, breathing problems, and certain cancers. BMI is intended as a tool for adults only, as children and adolescents are constantly growing so their weight-to-height ratios follow different patterns than adults who have achieved their full height.
The guide values for BMI are:
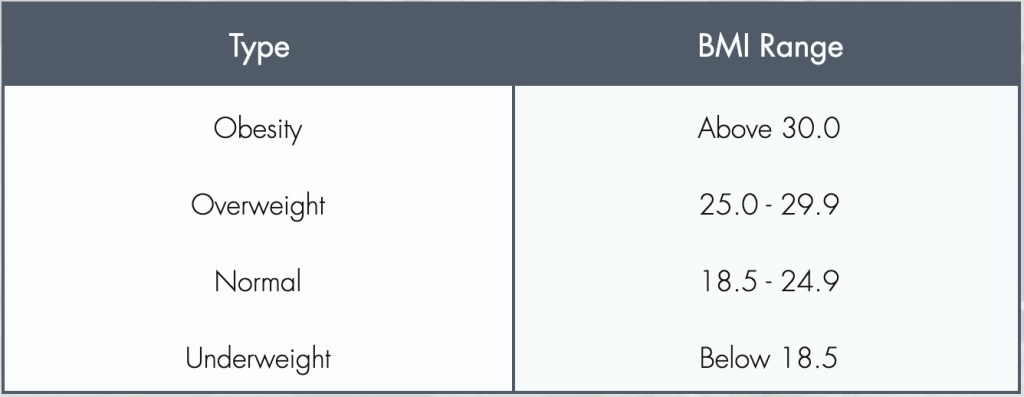
You should try to stay within the normal range. If you need help losing or gaining weight, you should talk with your doctor. Only your doctor has access to all your health measurements and can advise you on how to improve your BMI in a healthy way for you.
Pulse:
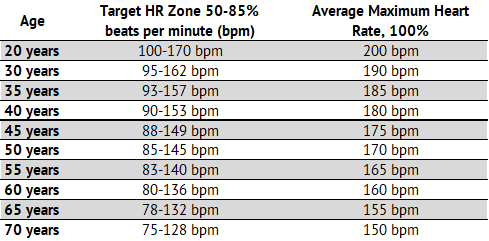
Pulse rate indicates the number of heartbeats per minute, reflecting heart rhythm and strength. A normal resting rate is typically between 60-100 beats per minute. Variations can signal heart conditions or general health issues.
Pulmonary Function Testing by Spirometry:
Pulmonary function tests are breathing tests to understand how well you move air in and out of your lungs. Spirometry is the most common test and measures how much air you can move into your lungs and how quickly you can move air out of your lungs. Spirometry can be used to diagnose respiratory conditions like asthma or chronic obstructive pulmonary disease (COPD). Wildfire smoke has high concentrations of particulate matter and irritants and can lead to lower lung function and exacerbate pre-existing respiratory conditions. Spirometry is one way to detect and help manage smoke-induced respiratory complications.
Your healthcare provider can use both your spirometry results, respiratory symptoms and other data to diagnose and treat lung disease. Spirometry provides a number of pulmonary function measurements:
Forced Vital Capacity (FVC):
FVC stands for the total amount of air you can forcefully exhale after taking a deep breath. It’s an important measure of how well your lungs work. If the FVC numbers aren’t within the normal range, it might mean there’s a problem with your lungs, like a disease that makes it hard to breathe in or out. But, remember, a low FVC result can also happen if you don’t blow out hard enough during the test.
Forced Expiratory Volume in 1 Second (FEV1):
FEV1 quantifies the volume of air expelled in the first second of a forced exhale. It’s crucial for assessing airflow obstruction. Decreased FEV1 may indicate conditions like asthma or COPD.
FEV1/FVC Ratio:
This ratio compares FEV1 to FVC to diagnose lung diseases. A reduced ratio suggests obstructive lung disease, while a normal or high ratio with reduced volumes indicates restrictive lung disease. If your levels are low, be sure to check this with your healthcare provider.
FEF25-75%:
FEF 25-75% evaluates air flow in the smaller airways. It can detect early changes before other measures. Abnormalities might suggest small airway disease.
Peak Expiratory Flow (PEF):
PEF tells us how quickly you can breathe out air at your fastest effort (fastest airflow rate during exhalation). It’s a good way to check on asthma or other issues that might be blocking your airways. Keep in mind, a low PEF reading might also happen if you don’t blow out hard enough during the test.
Blood Chemistry Tests (CHEM8+):
The CHEM8+ is a comprehensive blood chemistry panel that provides critical information on a patient’s metabolic status. This panel is essential for diagnosing and monitoring various health conditions, including kidney disease, diabetes, and electrolyte imbalances.
For wildfire survivors, the CHEM8+ panel is crucial for monitoring the effects of toxin exposure on metabolic functions. It assesses critical parameters like electrolytes, kidney function, and blood sugar levels, which can be impacted by inhaling harmful substances in wildfire smoke. This panel aids in early detection of potential health issues, for timely medical intervention.
Sodium (Na):
Sodium is key in maintaining fluid balance and nerve function. Normal levels range from 135-145 mmol/L. Abnormalities can indicate dehydration, kidney issues, or electrolyte imbalances.
Potassium (K):
Vital for cell function, especially in muscles. Normal values are 3.5-5.0 mmol/L. Deviations can signal kidney dysfunction or electrolyte disturbances.
Chloride (Cl):
Chloride helps maintain fluid balance and acid-base balance. Normal range is 96-106 mmol/L. Abnormal levels can indicate dehydration or kidney disease.
Total Carbon Dioxide (CO2):
Reflects kidney and lung function, and acid-base balance. Normal values are 23-30 mmol/L. Altered levels can suggest metabolic or respiratory issues.
Blood Urea Nitrogen (BUN):
Indicates kidney function and hydration status. Normal range is 5-24 mg/dL. High values can suggest kidney impairment or dehydration.
Ionized Calcium (iCa):
Important for bone health and muscle function. Normal range is 1.05-1.4 mmol/L. Abnormal levels can indicate parathyroid disorders, kidney disease, or bone disorders.
Creatinine (Crea):
Another marker of kidney function. Normal values vary by age, gender, and muscle mass. Normal range for males is 0.6 to 1.2 milligrams per deciliter (mg/dL). For the adult female, the normal range is 0.5 to 1.1 mg/dl. Elevated levels can indicate renal dysfunction.
Hematocrit (Hct):
Measures the proportion of red blood cells in blood. Normal range is 38.3-54% for men and 35.5-48% for women. Variations can indicate anemia or dehydration.
Hemoglobin (Hb):
Indicates the oxygen-carrying capacity of blood. Normal ranges are 13.8-18 g/dL for men and 12.1-16 g/dL for women. Abnormal levels can suggest anemia or polycythemia.
Anion Gap (AnGap):
Used to identify acid-base imbalances. Normal range is 3-12 mmol/L. Abnormal values can indicate metabolic acidosis or alkalosis.
CG4+ Test:
The CG4+ panel is primarily focused on assessing acid-base balance and respiratory status. It provides critical insights into respiratory and metabolic function, often used in critical care settings.
The CG4+ panel is important for evaluating the respiratory and acid-base balance in wildfire survivors. Exposure to smoke and airborne chemicals can lead to respiratory distress and metabolic imbalances. This panel helps in identifying and managing conditions like respiratory acidosis or alkalosis, for comprehensive health monitoring in the aftermath of wildfire exposure.
Lactate [mmol/L]:
Elevated lactate levels, beyond the normal range of 0.5-2.2 mmol/L, often indicate a lack of oxygen (hypoxia) or a condition where the body’s demand for oxygen exceeds supply. It’s a crucial marker in critical care, signaling metabolic stress or shock. Persistently high lactate levels can suggest severe organ dysfunction or failure. It’s also used to guide treatment strategies in critically ill patients.
pH:
The pH level in blood, ideally between 7.3-7.45, is a vital indicator of the body’s acid-base balance. Abnormal pH levels can have critical implications, with low pH indicating acidosis and high pH indicating alkalosis. These deviations can be due to respiratory or metabolic causes and are essential in diagnosing various health conditions.
Partial Pressure of Carbon Dioxide (PCO2) [mmHg]:
PCO2, normally within 40-60 mmHg, reflects the efficiency of ventilation. Elevated levels can indicate hypoventilation, while low levels suggest hyperventilation. PCO2 readings are integral in assessing respiratory function and managing conditions like COPD or asthma.
Partial Pressure of Oxygen (PO2) [mmHg]:
PO2 measures the oxygen level in blood, a normal range of 30-55 mmHg in venous blood. It’s used for evaluating lung function and oxygenation efficiency. Low PO2 can indicate respiratory issues like pneumonia, while high levels might be seen with supplemental oxygen therapy.
Total CO2 (TCO2) [mmol/L]:
TCO2, ranging between 23-29 mmol/L, is an important marker for evaluating the body’s acid-base status. It encompasses both bicarbonate and dissolved CO2 levels. Alterations in TCO2 levels can indicate metabolic disturbances or respiratory conditions.
Bicarbonate (HCO3) [mmol/L]:
Bicarbonate, typically 23-30 mmol/L in arterial blood, helps buffer the acids and bases in the body. It plays a significant role in maintaining the pH balance. Abnormal levels can indicate metabolic disorders or compensatory mechanisms in respiratory conditions.
Base Excess [mmol/L]:
Base excess, within the -2 to +2 mmol/L range, reflects the metabolic component of the body’s acid-base balance. It helps in diagnosing metabolic acidosis or alkalosis and guides the treatment of such imbalances.
Oxygen Saturation (sO2) [%]:
sO2, usually 40-85% in venous blood, indicates the percentage of oxygen-saturated hemoglobin. It’s a critical measure of respiratory and circulatory efficiency. Abnormal sO2 levels can signify respiratory distress or hypoxemia.
Disclaimer
The information on this page is for research only and not medical advice. Consult a healthcare professional for personal health concerns and interpretation of this data. Do not use this information as a substitute for professional medical evaluation and advice. Your health is important; always seek expert advice for a full understanding of your health.